The Peritoneum: Sensitivity, Abdominal Surgery, Adhesions, Breathing Exercises

Full disclosure. Three recent case studies. Two of the surgeries involved intra-abdominal surgery, and one was a DIEP flap surgery for reconstruction after a double mastectomy.
My husband had surgery for bowel cancer in October 2022. Care was good, and recovery was good. John performed both the breathing techniques and the ankle mobilisations the hospital gave. He was out of bed the morning after his surgery and built up to six miles of walking daily within a few weeks. I noticed a change in his posture; he has a slight stoop now. Altered posture could be the result of retiring, asymptomatic abdominal adhesions (more on this shortly) or sitting when he was having his chemotherapy as he developed extreme planter/palmar syndrome. It could be a combination.

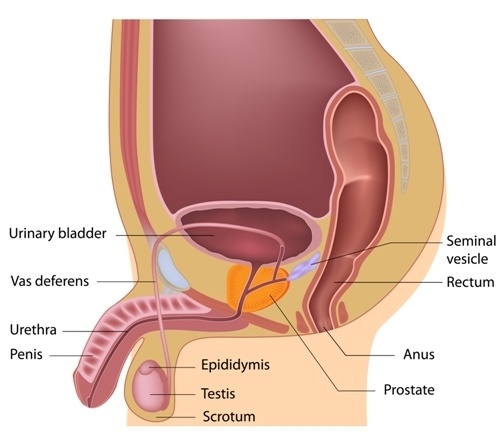
John has recently been diagnosed with prostate cancer. During the appointment to discuss treatment options, abdominal adhesions were raised. Any intra-abdominal surgery can result in abdominal adhesions. Adhesions can stick organs together and make it difficult for a surgeon to see clearly to perform further surgeries. They also increase the risk of damage to other structures. Surgery is not impossible; it requires more skill, in creased surgery length and associated complications.
I am currently treating a client for non-specific low back pain and pelvic pain; c-section six years ago. This client did not recall being given any breathing techniques post-surgery and did not do any specific pre or post-natal exercise sessions apart from the antenatal NHS course towards the end of her pregnancy.

My daughter has had reconstructive surgery using a DIEP flap after a double mastectomy. Her immediate care team did not give Debbie any breathing exercises; however, I gave her breathing techniques before her planned surgery, and when her consultant visited, he did talk about breathing. Debbie was encouraged to get out of bed soon after her surgery, and her care team gave no additional advice regarding movement apart from the exercise leaflet given to her in her pre-surgery pack.
I aim to remain objective in this text. I want to highlight the surrounding areas, pre-hab before surgery, the importance of breathing techniques to help with fluid dynamics and massaging and motility of abdominopelvic organs, client awareness and intention.
Peritoneum – Peri means around, and teino means to stretch
Peritoneum = stretched over
Location
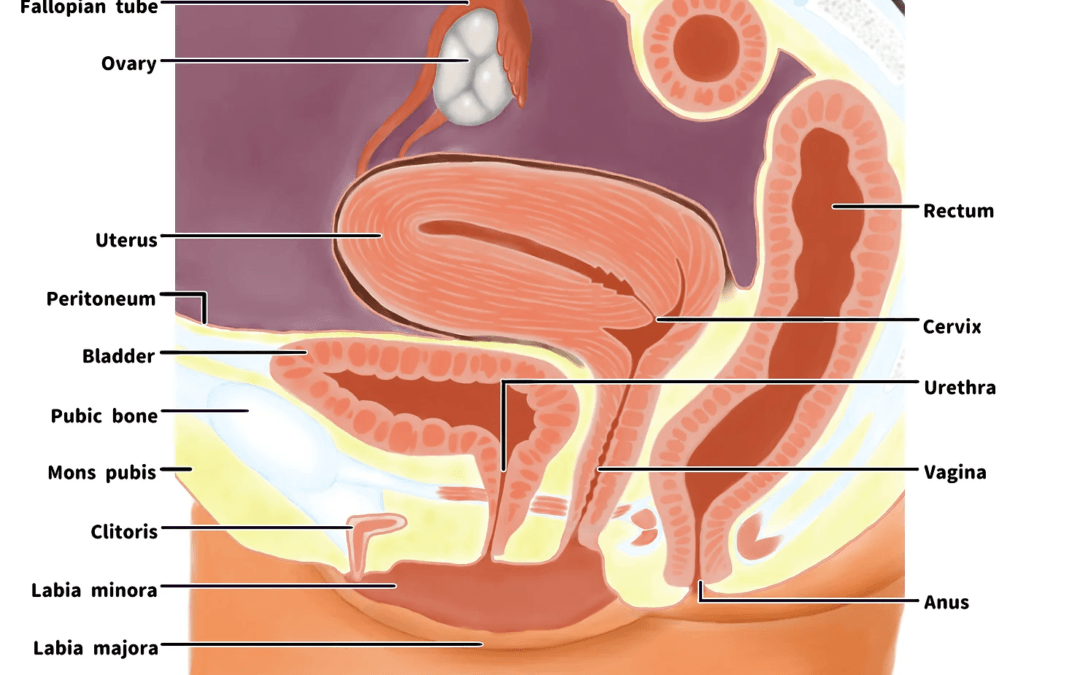
The peritoneum is located in the abdominopelvic cavity—the diaphragm above and the pelvic floor below.

Structure
-
Membranous structure. Two layers with a space between them. The two layers should slide on each other due to the lubricating fluid contained within. The area inside the two layers is the peritoneal cavity.
-
The boundaries of the peritoneal cavity include:- The abdominal muscles, the vertebrae, the pelvic floor, and the diaphragm. Many people divide the pelvic floor into three compartments. Note: Bordoni et al. add a fourth compartment, which includes the peritoneum, composed of the endopelvic fascia and perineal membrane. (Bookshelf ID: NBK482200)
-
The peritoneum supports the organs of the abdomen and serves as a fluid network for blood and lymph, and the nerves also need to navigate.
-
These membranes form the superficial parietal layer and the deeper visceral layer lining of the abdominal cavity.
-
The layers are continuous with each other. The parietal Peritoneun is the internal surface of the abdominopelvic walls. The parietal peritoneum is sensitive to pressure, pain, cutting, touch, friction and temperature. The deeper visceral layer is complex, developing into various folds and spaces with different names. These include the mesentery and omentum and the peritoneal ligaments and thickenings that help connect the visceral organs to each other and the walls to maintain the integrity of the peritoneal cavity. The visceral peritoneum is sensitive to stretch and chemical irritation.
-
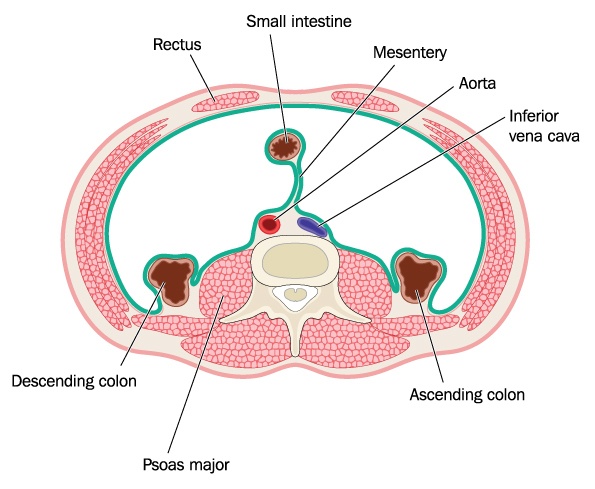
Note: Intraperitoneal organs, including the stomach, liver, and spleen, are covered front and back within the visceral peritoneum. The parietal peritoneum covers retroperitoneal (sub/infraperitoneal) organs below or behind the Intraperitoneal organs. Mnemonic that can help you remember retroperitoneal organs:- SAD PUCKER
-
S: Suprarenal (adrenal) gland
-
A: Aorta/Inferior Vena Cava
-
D: Duodenum (except the most proximal part, the duodenal cap)
-
P: Pancreas (except tail, this is the area that is towards the spleen)
-
U: Ureters
-
C: Colon (ascending and descending)
-
K: Kidneys
-
E: (O) Oesophagus
-
R: Rectum
Function
The layers contain fat, which helps protect your organs and regulate temperature. The peritoneal fluid lubricates the cavity and allows motion where needed. The arrangement of tissue and ligaments creates support and communication between your organs and anchors to the walls to stop unwanted movement. Blood, lymph vessels and nerves run through the layers of tissue. Your peritoneum is a protective barrier to injury and insults such as invasive particles and filters fluids in the peritoneal cavity.
Summed up -The peritoneum should provide a frictionless and protective barrier and allow for movement of the organs and tissues. It also has rapid healing properties.
According to Bordoni, there is a fourth compartment of the pelvic floor, the peritoneum composed of the endopelvic fascia and perineal membrane.

Disorders
I am listing some conditions and disorders. I will focus on my area of interest, abdominal adhesions: breath and movement.
Peritonitis – Inflammation of the peritoneum
Gastrointestinal diseases could appear as an infection in the peritoneal cavity and cause inflammation.
Ascites – A build-up of excess fluid in the peritoneal cavity. This excess fluid can result in abdominal swelling related to various diseases.
Hernia – mentioned because the organ involved will likely be wrapped in the peritoneum.
Abdominal adhesions:
Surgery that cuts through the peritoneum can cause bands of tough scar tissue to form. The incidence of postoperative adhesions is estimated to be about 67-93% (Sirovy et al., 2023). Other conditions that can lead to peritoneal injury with subsequent adhesions include radiotherapy, endometriosis, inflammation and local reactions to tumours (Sirvoy et al., 2023). The finding of post-laparotomy adhesions for the upper abdominal area is 93-100%, while for the lower abdominal area, it is around 67% to a maximum of 93% (Bordoni et al., 2023). Laparoscopic surgery has reduced problems with adhesions.
Although adhesions can be asymptomatic in a large proportion of patients who have undergone abdominal surgery, 3-20% require repeated hospitalisation within five years due to complications related to intra-abdominal adhesions.
Adhesiolysis, which treats the adhesions by cutting the adhesions surgically, is often the treatment of choice; this surgery creates a new adhesion in 80% of cases.
So, if I do not have any problems following abdominal surgery, what is the issue? Major previous abdominal surgery involving more than one quadrant may be considered a relative contraindication to robotic-assisted radical prostatectomy due to the increased risk of adhesions and bowel injuries and is often associated with longer operating time and increased blood loss (Duncan et al., 2019)
Adhesions are fibrous tissue connections that can stick two surfaces or organs together that are usually separate or limit normal motion in the cavity. Adhesions can indirectly cause pain or other symptoms like organ dysfunction by restricting organ motion; this creates tension and pulls on another organ or the walls of these cavities. Myelinated and non-myelinated nerve fibres developed within peritoneal adhesions; these fibres were more abundant in the abdominal than the pelvic adhesions (Struller et al. 2017).
Three risk factors are known to cause post-surgical adhesions (Fischer et al., 2020).
-
Abrasive damage to organ surfaces due to surgical mishandling.
-
Hypoxic pockets that develop at severed vessels and nerves.
-
Talcum powder irritation from surgical gloves.
Read the following review for further reading about medical strategies for preventing adhesions. Prevention of Post-Operative Adhesions: A Comprehensive Review of Present and Emerging Strategies. 2021
(Prostate cancer treatment with radiotherapyNote: NICE has now approved Barrigel, a hyaluronic acid spacer. This gel is inserted between the prostate and rectum before radiation therapy; this reduces the risks of radiation and adhesion formation as the rectum is moved away from the prostate. Although available on the NHS in the UK, your wait time for treatment will increase to around nine months at present, Jan 2024. It is available by private prescription at a cost of around £4000; you can then follow the general three-month hormone therapy before starting your prescribed dose of radiation.)
Adhesions develop as the body repairs in response to surgery, infection, trauma, or radiation and might resemble a thin sheet of plastic wrap or be a thick fibrous band. Any change in your norm could restrict movement and create abnormal stresses and tension between organs and tissues. The increase in stiffness or discomfort you feel after abdominal surgery could limit your movement and, if this is maintained, could lead to further adherence.
If we think back to the descriptor of peritoneum and the meaning of stretched over, we have a basis to begin. The tissues had a starting point, what they knew and how they felt and reacted pre-trauma.
-
We know that the peritoneal cavity sits below the diaphragm and thoracic cavity and is contained in the abdominopelvic cavity.
-
We have already mentioned a fourth compartment of the pelvic floor, which includes the peritoneum, composed of the endopelvic fascia and the perineal membrane.
-
The deeper layer of the pelvic floor is the endopelvic fascia and is linked with the pelvic viscera and levator ani muscle.
-
In abdominal surgery, it is common for adhesions to form. These could be local and or distal. They can be asymptomatic, and they can cause pain or dysfunction.
-
The mesentery is contained in the visceral peritoneum, and the root is attached to the back of the abdominal wall in front of the vertebrae at L1 to the right sacroiliac joint.
-
The diaphragm attaches to the ribs, and the abdominal muscles attach to the ribs. The diaphragm sits above the peritoneum. The rib cage should be able to expand as you inhale. The abdominal wall should be able to expand as you inhale. The diaphragm is connected with the liver, ascending colon, and duodenum, which are all part of the visceral peritoneum. The thoracolumbar fascia connects the pelvis from the sacrum to the neck and from the sacrum to the pelvic floor via the external anal sphincter. The cervical fascia from the neck becomes the endo thoracic fascia, joining the diaphragm and further along the transversalis fascia and transverse abdominus, internal obliques and beyond to the perineal membrane and levator ani of the pelvic floor.
-
The peritoneum is under constant stress from breathing, changes in blood and lymphatic flows, and movements from the trunk and abdomen (Bordoni et al., 2023).
-
Any disturbance in the synchronicity of the diaphragm and pelvic floor will result in intr-abdominal pressure changes and disturbing peritoneal drainage and organ motility.
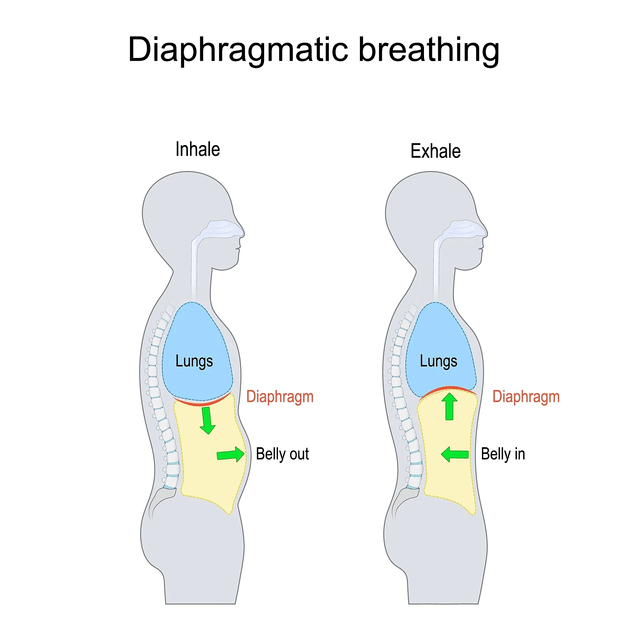
Quiet, functional breathing typically involves movement in the rib cage and the belly. The abdominal wound(s) and pain, muscle attachments and fascial connections may limit motion due to discomfort or lack of awareness. Unconscious postural adaptations to reduce tension or pain when sitting or moving around can create compression in the peritoneal cavity and, therefore, a lack of motility in the organs and tissues. Breathing patterns may alter or become dysfunctional over time.
How did I work with each of my case studies?
I went through the breathing exercises included in Johns’s pre-surgery information. We talked about the reasons for doing the exercises, including the cough. I asked him to relax his belly, feel it expand, and try not to slump when doing the exercises. I also gave him a variation of rhythmical breathing that could help with initial pain, including focusing on his heartbeat and a light wringing of a cloth between his hands. Once he was home, I included manual lymphatic drainage and gentle abdominal massage and looked at gait. John has started his pre-hab by starting pelvic floor sessions and breath-work with me. The NHS offer pre-hab for the pelvic floor for men having surgery as there is now lots of evidence regarding the benefits, it is not offered to those having hormone therapy and radiation. This is just one research paper – Pelvic floor muscles after prostate radiation therapy: morpho-functional assessment by magnetic resonance imaging, surface and digital anal palpation 2021 – doi:10.1590/S1677-5538.IBJU.2019.0765
It concludes: PFM functional assessment showed a decrease in sEMG activity in the Late group post-RT. Most of the sample group did not know how to actively contract the PFM or had weak voluntary contraction when assessed by digital anal palpation. Also these patients presented higher prevalence of pelvic complaints.
If the pelvic floor muscles are not functioning as they should, we now know that this does not just cause dysfunction locally. The respiratory and pelvic diaphragms work together and we know that Bordoni sees the peritoneum, perineal membrane and endo-pelvic fascia as a fourth layer of the pelvic floor. If the pelvic floor loses tone there could be a knock on with breathing. The peritoneal cavity is between these two diaphragms, the gentle stretch, compression that mobilises the tissues and is responsible for fluid dynamics and organ motility could change = pelvic complaints
For the lady with the C-section scar and pelvic and back pain, I have used Structural Integration and scar work in our face-to-face treatments and during Zoom sessions and homework, we are using a combination of Hypopressive Breathing, Pelvic Floor, Pilates, and self myofascial release making sure to incorporate positions and movements that seem to be an initiator of discomfort. This lady is not comfortable with seeing a women’s health physio but we are keeping the option open to explore visceral manipulation in the future.
Debbie is where I was better informed. I did some pre-hab with her. I got her to focus on her breathing and feel all areas. This gave her information and something to work towards after surgery. We included pelvic floor work as this would indirectly target the tummy. Deb was able to do diaphragmatic breathing, relax and expand the belly, and use focused rib cage breathing to target both areas of surgery. I also changed the intention for some breathing exercises to focus on the massage of the internal organs and fluid dynamics. All are gentle and non-invasive. Once home, she could continue breathing exercises during the day. She joined my breathing and pelvic floor sessions 2-4 times each week. Also, she followed the hospital exercise sheet (and believe it or not, she was only given exercises to support her recovery from the breast surgery). In week 4, we started Zoom sessions using the exercises from the hospital with the additional layer of playing with breathing, pelvic floor, and conscious engagement of the deep abdominals. We also refined her movements and started thinking about the tissue between the surgeries and beyond, and she joined my hypopressive postural breathing sessions. Debbie has done the Pink Ribbon Breast Cancer Post Surgery Rehab Programme with me via Zoom and continues to do this. She has walked from day one and now walks 3-5 miles daily. She has gone back to work just under three months after her operation. It is not all healed; she has become allergic to the stitches, and some of the wounds are still open in places.
As you can see, I have used breathwork in all three case studies. Breathing techniques improve overall health. They are gentle, and you change the intention of a specific area or awareness and even the position to apply different tensions into the tissues or organs. The use of breath changed the stretched over tension and pressure of the peritoneal cavity to influence the tissue, organs, and fluid dynamics. Awareness and education before surgery give the patient confidence in what they are doing. Breathing exercises calm the mind, improve digestion, reduce anxiety and gently mobilise the tissue and organs. I think the different pre- and post-care care each of these case studies received also highlights the need for standard practices in the UK among different medical boards and even internally amongst staff.
I have since found these research papers.
Deep breathing exercise education receiving and performing status of patients undergoing abdominal surgery. International Journal of Health Sciences 2018. Results: 56% of patients received education about deep breathing exercises, and 51.5% performed them. Nearly half of those given the exercises received them after surgery. Concludes: Surgical patients did not receive adequate education about deep breathing exercises; most received this education after their surgeries. As a promising finding, receiving education affected patients’ exercise performance status positively.
Effectiveness of Rhythmic Breathing Exercise on Postoperative Pain among Patients Undergone Major Abdominal Surgery in MGMCRI at Puducherry, India 2019 – Concludes: Prevalence of postoperative pain is most common among patients undergoing major abdominal surgery. Rhythmic breathing exercises reduce postoperative pain and improve levels of physical functioning. It does not show any side effects, improves quality of life and is easy to do.
Balancing the Diaphragms – Using the pelvic and respiratory diaphragms we influence the peritoneal cavity
Sometimes treatment requires a multidisciplinary approach. It is very often a jigsaw and requires lots of reading and research, digging and diving down new rabbit holes. I absolutely encourage anyone needing surgery to do your research and do some pre-hab. Please contact me if you have questions.