I have often heard the prostate described as a walnut-sized gland. However, I think I get a different sense with ping-pong sized, rubbery gland. I have also heard it referred to as an inverted cone. I often say words matter, and perhaps we should have other ways to talk to our clients when describing body parts. A library of words, sentences, and paragraphs fit different scenarios and clients.
A high percentage of men are unaware they have a pelvic floor and unaware of the prostate until something is wrong with it. A study of risk factors and knowledge of the pelvic floor muscles in Norwegian powerlifters concluded that pelvic floor dysfunction was high and that athletes had limited understanding of the pelvic floor muscles. Seventy-four percent of the men taking part did not know why they should train the pelvic floor, and seventy-two and a half percent did not know how to train them.
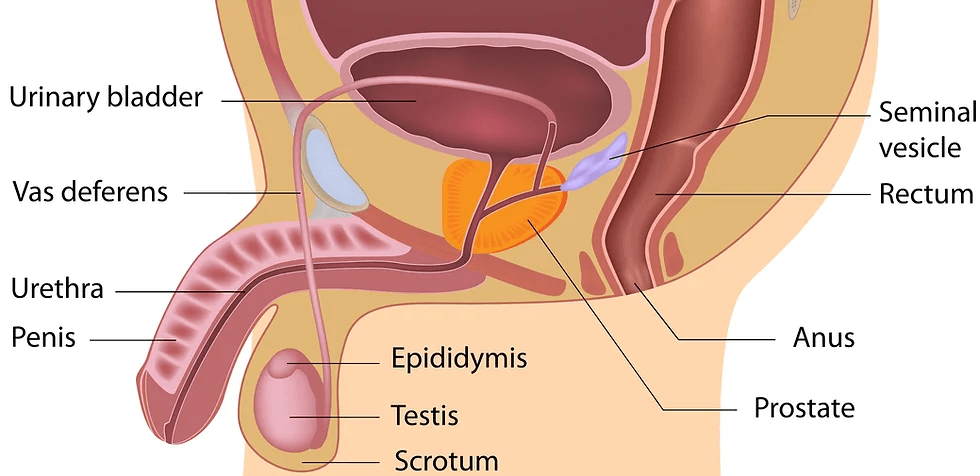
The prostate is part of the male reproductive system; it sits below the bladder and produces semen.
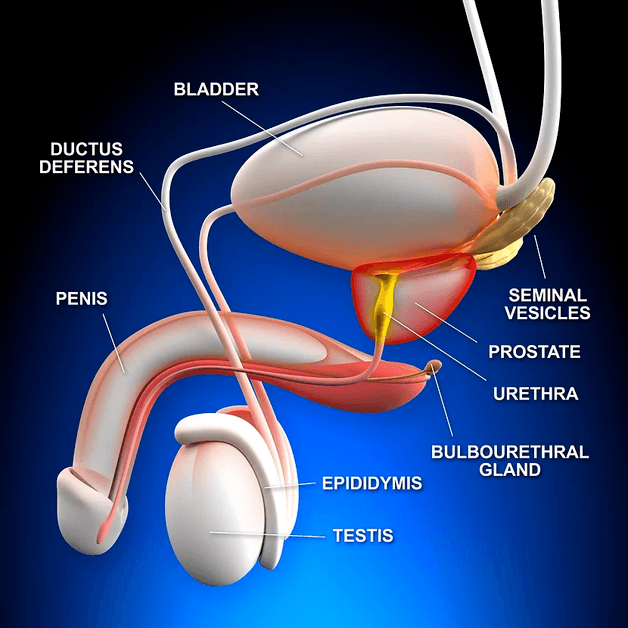
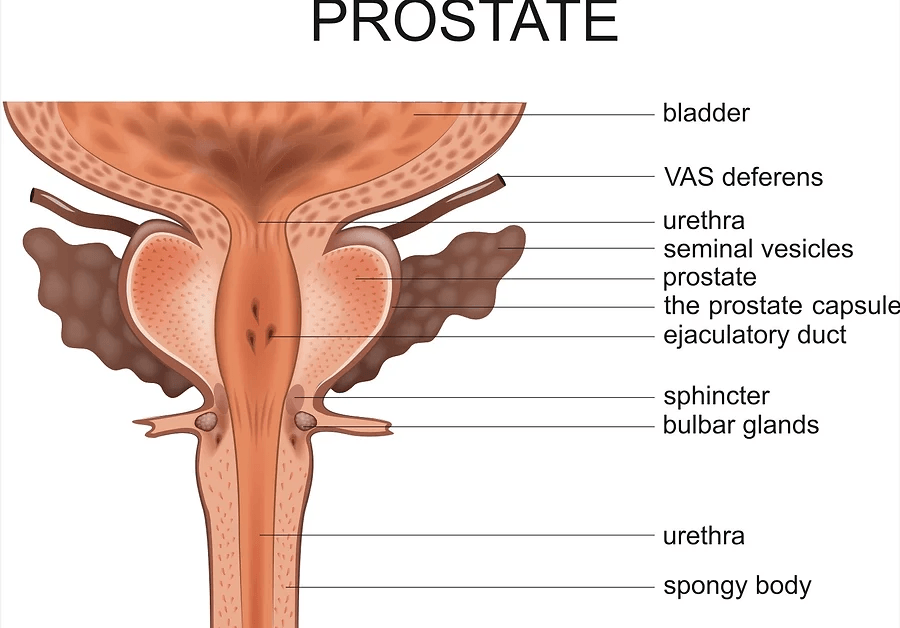
Let’s look at the prostate as an inverted cone to see how the prostate is situated. The prostate base is located at the top, much of it connecting to the bottom of the bladder. The apex rests on the perineal membrane. The external urethral sphincter wraps around the urethra as it exits the prostate to control ejaculatory and urinary flow. The levator ani muscles attach to the sides. The posterior wall of the prostate is separated from the rectum by denonvilliers fascia. The anterior surface is behind the lower part of the pubic bone and attached to the pubic bones by the puboprostatic ligaments.
The prostate is encapsulated in an outer false capsule known as the prostatic sheath and is a continuation of the pelvic fascia and the inner capsule. These surround the prostatic venous plexus (also known as Santorini’s plexus); this network of veins drains the prostate gland into the internal iliac veins.
If we cut the prostate through the centre and lifted the top off, we would see more of the walnut or chestnut description and identify different lobes: two larger, lateral lobes, one on each side; this is often where enlargement of the ageing prostate found. In addition, there is an anterior lobe (sometimes known as the Isthmus) directly in front of the urethra, two ejaculatory ducts, a median lobe directly behind the urethra, and a posterior lobe that sits slightly below the ejaculatory ducts.
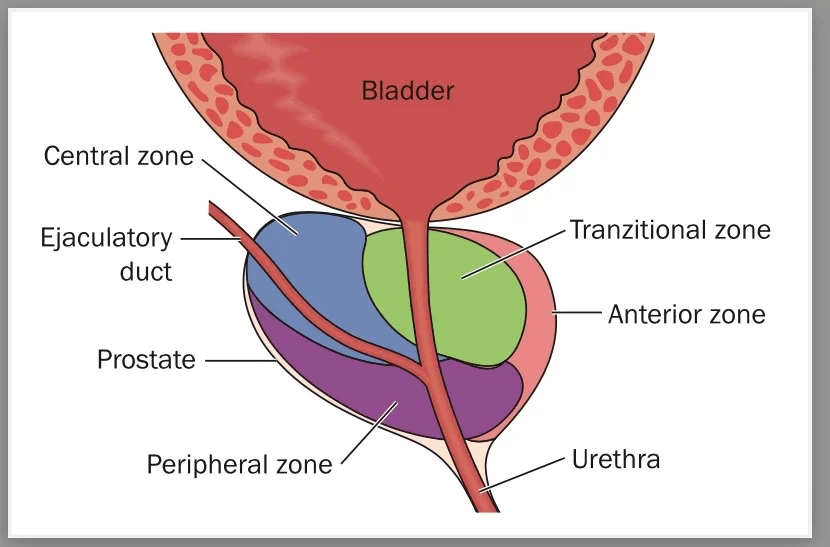
We can also look at the prostate clinically in zones according to their function—the central zone surrounding the ejaculatory ducts and the peripheral zone, which covers much of the central zone and is also the largest. A transitional or glandular zone surrounds a portion of the urethra between the urinary bladder and seminal colliculus (verumontanum). This zone is just distal to the ejaculatory ducts on either side. Finally, the fibromuscular stroma is the area of the prostate anteriorly that could be described as a fourth zone.
Functions: The prostate helps produce semen from the sperm the testicles emit. Thick mucus-like fluid from the bulbourethral gland (Cowper’s gland) below the prostate helps to neutralise the acidic urine in the urethra. The prostate produces Prostatic -Specific antigen ((PSA) – high levels of this can indicate prostate cancer). The prostate helps to pump out the sperm during intercourse. The prostate also acts as a filter to remove toxins, meaning that if the air that we breathe and the food we eat are not good, it has to work harder. The prostate nerves help create and maintain erections. Secretions from the prostate can help protect against urinary tract infections. It controls urine flow down the urethra and ensures urine and sperm do not get mixed when a man ejaculates. The male hormones dihydrotestosterone result from testosterone being converted to DHT by the 5-alpha reductase enzyme in the prostate; this hormone is responsible for the male sex drive.
All that from a gland that weighs about 30 grams!
Anatomy, Abdomen and Pelvis, Prostate – https://www.ncbi.nlm.nih.gov/books/NBK540987
Prevalence of Pelvic Floor Dysfunction, Bother and Risk Factors of the Pelvic Floor Muscles in Norwegian Male and Female Powerlifters and Olympic Weightlifters – 2020 DOI: 10.1519/JSC.0000000000003919
