One of my favourite jobs is delivering pelvic health introduction workshops, a safe place to discuss the common problem of having a weak pelvic floor.
Do you have a good pelvic floor?
If you want to monitor your pelvic floor health, below are some questions to help you. Collecting this information over a few days or up to a week will be a way to start the conversation with your GP or Physio.
Pelvic Floor Tracker
How often do you pee in 24 hours? Day_______ Night______
Do you need to go at the first sensation?
When you have the urge to pee, do you have time to get to the toilet?
Do you feel the urge to pee again as soon as you have been?
Do you leak when you laugh, cough, sneeze or jump?
Do you have a heavy sensation low in the pelvis? It might feel like something is pushing down or falling out.
If you examine yourself, can you see or feel anything?
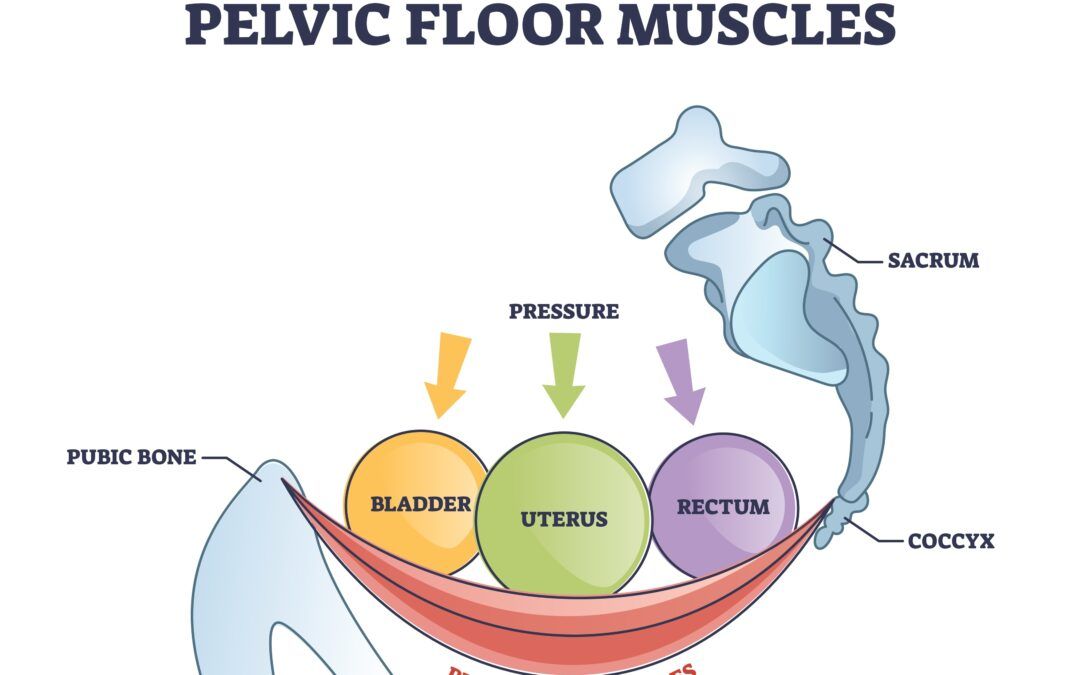
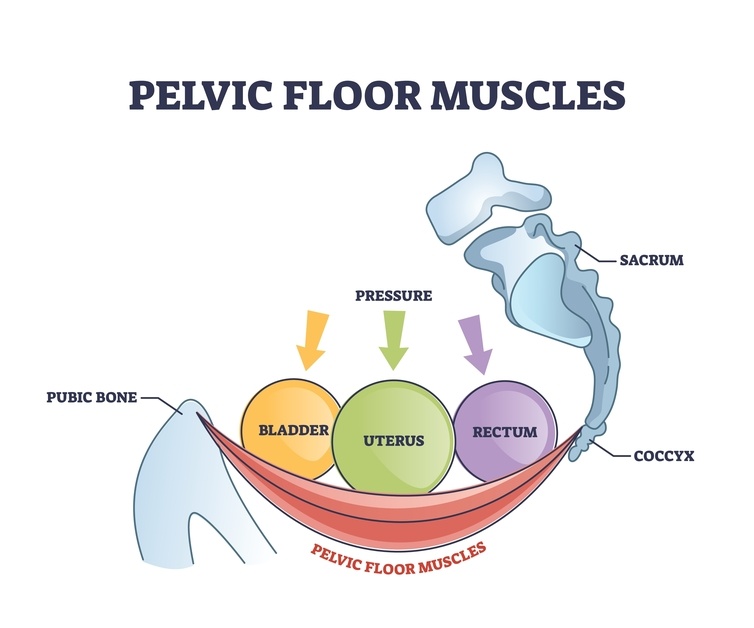
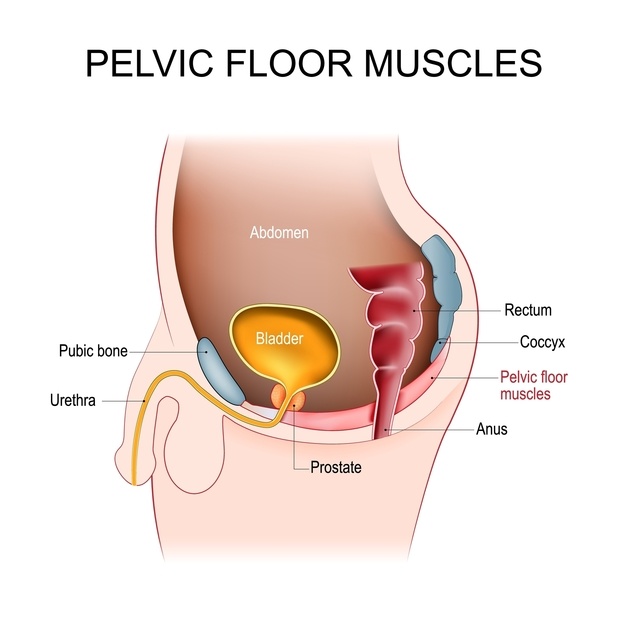
Functions of the pelvic floor muscles
-
Supporting the organs. In women, the bladder, uterus and rectum
-
Control of the bladder and bowel, allowing us to pass urine and faeces. We can control our external anal sphincter.
-
Sexual function. A well-functioning pelvic floor can improve your sex life.
-
Circulation. The muscles will help with fluid dynamics, acting as a pump. It works in synergy with the respiratory diaphragm.
-
Postural stability. Improve your balance to help support your pelvic floor. Pelvic floor muscle training is part of training your core as a system and supports the spine and pelvis
Just a little geeky anatomy – My favourite muscle of the pelvic floor group – Puborectalis
Some Statistics
This description covers various symptoms relating to pelvic floor function and musculature.
-
60% of women report at least one symptom of poor pelvic health when questioned.
-
85% of adults with faecal incontinence have not been to the GP.
-
50% of adults with an overactive bladder (sudden urge) are not seeking help.
-
20% of men under 40 and 50% of men over 40 have erectile dysfunction.
-
Up to 70% of men suffer from urinary incontinence following prostatectomy surgery.
-
A study in 2018 found that over 95% of women with low back or pelvic pain had some form of pelvic floor dysfunction. 66% had pelvic floor weakness.
-
52% of women who seek help for pelvic floor dysfunction are found to have pelvic organ prolapse.
-
Are you one of the 46% living with a pelvic floor problem for up to 5 years without seeking help?
Pregnancy
-
Around 1 in 3 women experience urinary incontinence three months after pregnancy, and 1 in 12 women report symptoms of pelvic organ prolapse.


Pelvic Floor Muscle Training
-
Around 25% of women have never done pelvic floor exercises that could prevent or improve their symptoms.
-
Over half the women surveyed were not currently doing pelvic floor exercises.
-
23% do not know how to do pelvic floor exercises.
-
Only 22% of women do regular pelvic floor muscle training.
-
Pelvic floor muscle training is a conservative treatment that can effectively improve symptoms of pelvic floor dysfunction.
-
Supervised pelvic floor muscle training is associated with better symptom improvement.
-
A 121 session with a health professional can prove very beneficial as a programme can be tailored to you.
-
Join a class to learn the correct techniques and build the consistent habit of training muscles you can’t see.
-
Consistency is vital; it can take three to four months to notice the benefits.
-

Outlay and choices for clients
-
NHS services. In 2018/19, it was estimated that community health services charged £54 for group physiotherapy or £63 for individual sessions, based on one hour weekly for a set number of weeks.
-
If you access NHS services for pelvic floor muscle training at the end of the programme, you should continue this training as consistency is key. The pelvic floor gym! There are many programmes out there. I recommend Adore Your Pelvic Floor and Diamond Pilates.
-
I also recommend Hypopressure low-pressure breathing and exercise as an additional component of overall core health. I run online sessions; you can find more information through
-
Supervised pelvic floor muscle training is a cost-effective and conservative treatment. It reduces the long-term risk of requiring hospital-based therapy for pelvic floor disorders. Regular pelvic floor muscle training provides symptom relief and improves the quality of life among women with urinary incontinence.
Below are links to articles and research papers if you’d like to learn more about the pelvic floor and its effects on the body.
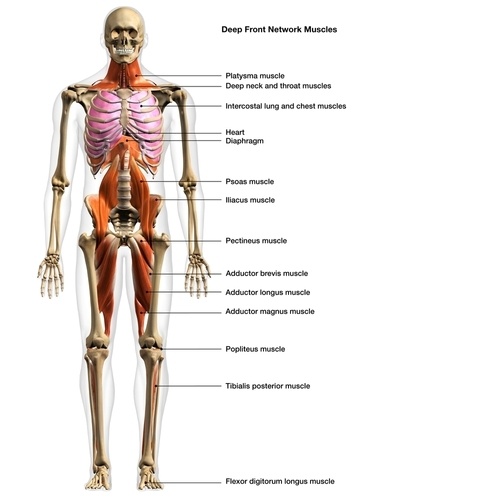
And let’s remember the feet, the tongue and our deep front line.
-
Foot pronation affects pelvic motion during the loading response phase of gait.
-
This is my favourite research article; it is long, and everyone can learn something from it. You can appreciate the relationships from one part of the body to another. The most common functional disorders and factors affecting female pelvic floor.
A topic that has never come up before. There has been a rise in the popularity of anal sex among teenagers. I have done a little research; studies state 16-24 years. However, I have asked colleagues who are talking, even 12-13 years. The reason kids say they are doing it is not to get pregnant. There has been a rise over the last decades from 12.5% of people having anal intercourse to 28.5%. Studies show that anal intercourse is linked to increased risk of faecal incontinence.
Women have a weaker anal sphincter to start with; add to this that the girl might not be relaxed as they are not fully happy about what they are doing. It can cause injury to the sphincter, resulting in faecal incontinence, especially if performed multiple times. Informed consent: maybe it is time to talk with our teens and tell them the pros and cons. Social media or playground gossip might only portray the racy side.
I am passionate about getting people to move without pain and empowering people to help themselves by educating them.